Implementing Telehealth Visits
March 20th, 2020 - NamasCategories: Primary Care|Family Care CPT® Coding Diagnosis Coding HCPCS Coding Modifiers ENT|Otolaryngology
The following is a step-by-step guide on how to convert office-based encounters to telehealth encounters during the current COVID-19 pandemic. These rules may change post-pandemic, as many changes relaxing existing rules were made on a temporary basis by CMS and commercial payers to facilitate patient access and minimize risk of infection.
Step 1: Telehealth Consent
In order to conduct a patient encounter as a telehealth service, the patient must consent to this modality. The consent should include the patient's explicit agreement to being treated via telehealth rather than in a face-to-face encounter.
Each consent form should include the following elements:
- Patient name and date of birth
- Date of service
- Rendering provider
- Elect services as a telehealth encounter
- Instructions regarding the proper location for the patient during the telehealth encounter
- Patient vs. provider responsibilities in case of technical difficulties
- Payment considerations
- Signature or verbal attestation by the patient
The consent form for each patient should be retained permanently in their record. Examples of Telehealth Consent Forms are found on the NAMAS COVID-19 Resource Page.
Step 2: Scheduling
The patient should be scheduled for their telehealth encounter. If transferring from an in-person visit to a telehealth visit, maintaining the same schedule maybe appropriate. Telehealth visits may be used to care for existing patients with acute concerns or ongoing management of chronic conditions. These services and associated relaxations of telehealth rules are not limited to patients with confirmed or suspected COVID-19. Prior to scheduling, front office staff should:
- Prep charts as usual
- Issue appointment reminders to each patient
- Ensure telehealth consent is on file
Step 3: Telehealth Encounter
The rendering provider should contact the patient through electronic means. The provider may use a HIPAA-compliant, secure telehealth service/program, such as Doxy.me or VSee, although HHS has stated they will not penalize physicians who use non-HIPAA compliant software such as Skype, FaceTime, or Google Meetings.
The rendering provider should also take some extra steps for telehealth encounters:
- While HIPAA guidelines have been "relaxed" during the pandemic, the provider should make every effort to ensure that the telehealth encounter is conducted in a secure area to maintain patient privacy.
- Rendering providers should keep the telehealth interface open and ready for the patient to join the session.
- Upon entering the telehealth "exam room," the provider should consider reminding the patient of the following:
- During this telehealth encounter medical care may be impacted by communication and therefore, the patient is encouraged to be as transparent and blunt about their concerns and complaints as possible.
- Remind the patient that while the provider is taking precautions to ensure privacy as required by HIPAA, the patient's surroundings also pose risks of a HIPAA breach for which the provider/organization cannot be responsible.
- Inform the patient that active treatment and care is being provided during the encounter for their presenting problem, but further workup, testing, treatment, or aftercare is the responsibility of the patient. Non-urgent healthcare services at this time may not be a high priority for referral organizations and therefore the patient may have to make an increased effort to ensure treatment plans are followed.
- The provider should document the encounter as they would a normal, in-person office visit.
- History, to include CC, HPI, ROS, and PFSH should be included as these are all subjective, obtainable through the online interview process with the patient.
- Exams will be limited, but providers are encouraged to consider what is appropriate and medically indicated. Keep in mind that not every patient requires an 8-point organ system exam. Most telehealth patients will support E/M services represented by codes 99212, 99213, or 99214 and therefore the ONLY exam elements required per 1995 documentation guidelines are:
- 99212 - 1 organ system (this could merely be a general statement of the patient's appearance)
- 99213 - 2 organ systems
- 99214 - 2 organ systems with the affected organ system including 3-4 findings. This level of exam may prove difficult in the telehealth setting
- Assessment and plan, which includes the provider's clinical assessment of the complexity of the patient's condition, and a plan of treatment must be included and would not be compromised by the telehealth setting. If the assessment may be limited based on the need for additional workup, this should be noted in the documentation.
Step 4: Selecting the appropriate reportable service
Reporting the service varies by payer. It is advisable to have the providers focus on rendering and documenting the service, allowing the staff to choose the appropriate reportable codes.
ICD-10-CM diagnosis coding considerations:
Guidance from the American Academy of Family Practitioners (AAFP) calls for using either J12.89 (other viral pneumonia) or B97.29 (other coronavirus as cause) as the diagnosis code for confirmed COVID-19. Note B97.29 is a supplementary code to identify a primary manifestation of COVID-19 and should not be the first-listed code. For suspected COVID-19, report ICD-10 codes for the presenting signs and symptoms. For known exposure to COVID-19 without definitive diagnosis, report Z20.828; for suspected exposure that is ruled out after exam, report Z03.818.
(Click for larger image)
Modifiers for Consideration:
- GQ: Asynchronous telehealth service.
- 95: Synchronous telemedicine service rendered via real-time interactive audio and video telecommunications system.
- GT: Critical Access Hospital (CAH) distant site providers billing under CAH Optional Method II*. This goes on an institutional claim and pays 80% of the professional fee schedule rate.
- G0 (zero): Used to identify telehealth services furnished for purposes of diagnosis, evaluation, or treatment of symptoms of an acute stroke (see below).
- GY: Notice of Liability Not Issued, Not Required Under Payer Policy. Used to report that an Advanced Beneficiary Notice (ABN) was not issued because item or service is statutorily excluded or does not meet definition of any Medicare benefit.
*CAH payment method II allows CAHs to receive cost-based payment for facility services, plus 115% of fee schedule payment amount for professional services.
CMS offers special rules for telehealth services furnished to patients who have suffered an acute stroke. Beginning on Jan. 1, 2019, telehealth services furnished for purposes of diagnosing, evaluating, or treating the symptoms of an acute stroke do not have the usual restrictions on geographic locations and the types of originating sites associated with normal telehealth services.
To indicate such a service, the new informational HCPCS modifier G0 should be appended to the reported codes. Modifier G0 is valid for all telehealth distant site codes billed with Place of Service (POS) code 02 or critical access hospitals, CAH method II (revenue codes 096X, 097X, or 098X). The modifier should also be reported with the telehealth originating site facility fee code Q3014 (see below).
Place of Service (POS) Codes for Consideration:
Use POS code "02" (telehealth) for all telehealth services reported to Medicare. For commercial payers, POS "02" may not be required, but the appropriate telehealth modifier is instead required. The most common telehealth modifier for commercial payers is -95.
Step 5: Keep it Simple
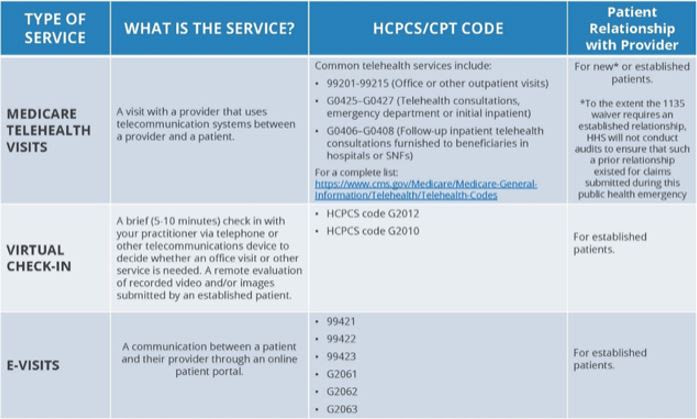
Most carriers are allowing relaxation for telehealth services to utilize the E&M services codes in lieu of the telehealth codes. This will make coding selections seamless for the provider and their coding team. The table below was published by CMS this week to provide such guidance.
###
Questions, comments?
If you have questions or comments about this article please contact us. Comments that provide additional related information may be added here by our Editors.
Latest articles: (any category)
Artificial Intelligence in Healthcare - A Medical Coder's PerspectiveDecember 26th, 2023 - Aimee Wilcox
We constantly hear how AI is creeping into every aspect of healthcare but what does that mean for medical coders and how can we better understand the language used in the codeset? Will AI take my place or will I learn with it and become an integral part of the process that uses AI to enhance my abilities?
Specialization: Your Advantage as a Medical Coding ContractorDecember 22nd, 2023 - Find-A-Code
Medical coding contractors offer a valuable service to healthcare providers who would rather outsource coding and billing rather than handling things in-house. Some contractors are better than others, but there is one thing they all have in common: the need to present some sort of value proposition in order to land new clients. As a contractor, your value proposition is the advantage you offer. And that advantage is specialization.
ICD-10-CM Coding of Chronic Obstructive Pulmonary Disease (COPD)December 19th, 2023 - Aimee Wilcox
Chronic respiratory disease is on the top 10 chronic disease list published by the National Institutes of Health (NIH). Although it is a chronic condition, it may be stable for some time and then suddenly become exacerbated and even impacted by another acute respiratory illness, such as bronchitis, RSV, or COVID-19. Understanding the nuances associated with the condition and how to properly assign ICD-10-CM codes is beneficial.
Changes to COVID-19 Vaccines Strike AgainDecember 12th, 2023 - Aimee Wilcox
According to the FDA, CDC, and other alphabet soup entities, the old COVID-19 vaccines are no longer able to treat the variants experienced today so new vaccines have been given the emergency use authorization to take the place of the old vaccines. No sooner was the updated 2024 CPT codebook published when 50 of the codes in it were deleted, some of which were being newly added for 2024.
Updated ICD-10-CM Codes for AppendicitisNovember 14th, 2023 - Aimee Wilcox
With approximately 250,000 cases of acute appendicitis diagnosed annually in the United States, coding updates were made to ensure high-specificity coding could be achieved when reporting these diagnoses. While appendicitis almost equally affects both men and women, the type of appendicitis varies, as dose the risk of infection, sepsis, and perforation.
COVID Vaccine Coding Changes as of November 1, 2023October 26th, 2023 - Wyn Staheli
COVID vaccine changes due to the end of the PHE as of November 1, 2023 are addressed in this article.
Medicare Guidance Changes for E/M ServicesOctober 11th, 2023 - Wyn Staheli
2023 brought quite a few changes to Evaluation and management (E/M) services. The significant revisions as noted in the CPT codebook were welcome changes to bring other E/M services more in line with the changes that took place with Office or Other Outpatient Services a few years ago. As part of CMS’ Medicare Learning Network, the “Evaluation and Management Services Guide” publication was finally updated as of August 2023 to include the changes that took place in 2023. If you take a look at the new publication (see references below),....