
Reporting Tooth Numbers and Oral Cavity Areas
February 1st, 2018 - Chris Woolstenhulme, QCC, CMCS, CPC, CMRS
When billing for dental procedures you need to identify the exact tooth and/or location in the oral cavity. Qualifiers are used to report the location and tooth number. When billing procedures on teeth and the oral cavity, the JP qualifier is used to identify the tooth number(s) and the JO qualifier is used to report the area of the oral cavity. National Uniform Claim Committee (NUCC) states to report the qualifiers and tooth numbers in the following order.
-
Qualifier
-
Area of oral cavity
Example: J010
When reporting multiple tooth numbers for one procedure report in the following order
-
Qualifier
-
Tooth Number
-
Blank Space
-
Tooth number
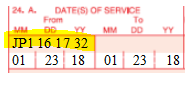
Example: JP1 16 17 32
When reporting multiple areas of the oral cavity for one procedure, add in the following order: qualifier, oral cavity code, blank space, oral cavity code, etc., e.g., JO10 20.
When reporting multiple areas of the oral cavity for one procedure, the number of units reported in 24G is the number of areas of the oral cavity involved in the procedure.
JP Qualifier
The following are the codes for tooth numbers and are reported with the JP qualifier:
-
1 – 32 Permanent dentition
-
51 – 82 Permanent supernumerary dentition
-
A – T Primary dentition
-
AS – TS Primary supernumerary dentition
JO Qualifier
The following are the codes for areas of the oral cavity, reported with the JO qualifier:
-
Entire oral cavity
-
Maxillary arch
-
Mandibular arch
-
10 Upper right quadrant
-
20 Upper left quadrant
-
30 Lower left quadrant
-
40 Lower right quadrant
This information is entered in Box 24 in the gray area above the Date of Service.
###
Questions, comments?
If you have questions or comments about this article please contact us. Comments that provide additional related information may be added here by our Editors.
Latest articles: (any category)
Artificial Intelligence in Healthcare - A Medical Coder's PerspectiveDecember 26th, 2023 - Aimee WilcoxWe constantly hear how AI is creeping into every aspect of healthcare but what does that mean for medical coders and how can we better understand the language used in the codeset? Will AI take my place or will I learn with it and become an integral part of the process that uses AI to enhance my abilities?
Specialization: Your Advantage as a Medical Coding ContractorDecember 22nd, 2023 - Find-A-CodeMedical coding contractors offer a valuable service to healthcare providers who would rather outsource coding and billing rather than handling things in-house. Some contractors are better than others, but there is one thing they all have in common: the need to present some sort of value proposition in order to land new clients. As a contractor, your value proposition is the advantage you offer. And that advantage is specialization.
ICD-10-CM Coding of Chronic Obstructive Pulmonary Disease (COPD)December 19th, 2023 - Aimee WilcoxChronic respiratory disease is on the top 10 chronic disease list published by the National Institutes of Health (NIH). Although it is a chronic condition, it may be stable for some time and then suddenly become exacerbated and even impacted by another acute respiratory illness, such as bronchitis, RSV, or COVID-19. Understanding the nuances associated with the condition and how to properly assign ICD-10-CM codes is beneficial.
Changes to COVID-19 Vaccines Strike AgainDecember 12th, 2023 - Aimee WilcoxAccording to the FDA, CDC, and other alphabet soup entities, the old COVID-19 vaccines are no longer able to treat the variants experienced today so new vaccines have been given the emergency use authorization to take the place of the old vaccines. No sooner was the updated 2024 CPT codebook published when 50 of the codes in it were deleted, some of which were being newly added for 2024.
Updated ICD-10-CM Codes for AppendicitisNovember 14th, 2023 - Aimee WilcoxWith approximately 250,000 cases of acute appendicitis diagnosed annually in the United States, coding updates were made to ensure high-specificity coding could be achieved when reporting these diagnoses. While appendicitis almost equally affects both men and women, the type of appendicitis varies, as dose the risk of infection, sepsis, and perforation.
COVID Vaccine Coding Changes as of November 1, 2023October 26th, 2023 - Wyn StaheliCOVID vaccine changes due to the end of the PHE as of November 1, 2023 are addressed in this article.
Medicare Guidance Changes for E/M ServicesOctober 11th, 2023 - Wyn Staheli2023 brought quite a few changes to Evaluation and management (E/M) services. The significant revisions as noted in the CPT codebook were welcome changes to bring other E/M services more in line with the changes that took place with Office or Other Outpatient Services a few years ago. As part of CMS’ Medicare Learning Network, the “Evaluation and Management Services Guide” publication was finally updated as of August 2023 to include the changes that took place in 2023. If you take a look at the new publication (see references below),....

